The SARS-CoV 2 virus can affect different types of body cells, and the end of the acute phase does not always mean complete recovery of the patient, because it is now known that coronaviruses can persist in the cells of the nervous system for a long time. The term “chronic” or “long-term” infectious process implies persistence of the pathogen. According to the terminology of the Infectious Diseases Society of America (IDSA), such phenomenon is described as “Long COVID”, “post-COVID syndrome” and “post-acute COVID-19 syndrome”, while Harvard Medical School uses the term “long-hauler”.
Acute COVID-19: signs and symptoms of COVID-19 for up to 4 weeks.
Ongoing symptomatic COVID-19: signs and symptoms of COVID-19 from 4 to 12 weeks.
Post-COVID-19 syndrome: signs and symptoms that develop during or after an infection consistent with COVID-19, continue for more than 12 weeks and are not explained by an alternative diagnosis.
Post-COVID long-hauler – a person diagnosed with COVID-19 caused by SARSCoV 2 who has not returned to baseline health and body functioning 3 to 6 months after the illness.
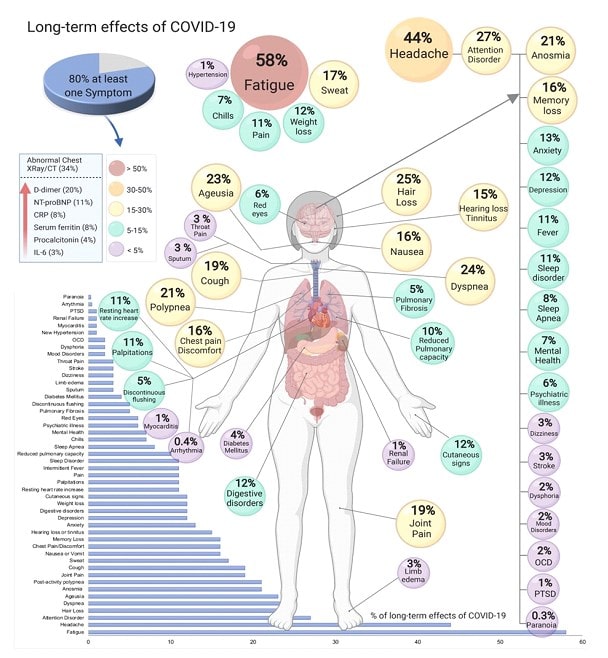
According to various estimates, 10 to 50% of patients who have had COVID 19 become “long-hauler”: some of these patients have irreversible damage to the lungs, heart, kidneys, or brain that impairs the functioning of these organs; others, despite no noticeable organ damage, still have debilitating symptoms.
Long-COVID hides under different masks: scientists identify more than 200 post-COVID symptoms in 10 organ systems. Long-COVID-19 masks have a common pathogenesis of complications – pathophysiological syndromes: endotheliitis, systemic inflammation, pulmonitis and a pronounced clinical syndrome – asthenia.




After acute COVID 19 requires mandatory monitoring of respiratory function, cardiac symptoms, nervous system and mental functions, as well as syndrome-pathogenetic approach to patient rehabilitation, aimed primarily at eliminating systemic background inflammation, improving endothelial function.
Multidisciplinary inpatient rehabilitation is recommended for maximum recovery in patients with moderate or severe post-covid symptoms.